Do you have your Advance Health Care Directive (Living Will)?
I was a hypocrite! Years ago, during my caregiver keynote speeches, my advice to caregiving families was to complete their own estate plans and help their parents and other loved ones complete theirs. One audience member bravely asked if I had completed mine. “No,” I replied feeling flush. To save face, I added, “I’m only 38.” That was 22 years ago; I realized shortly thereafter that I had to draft my estate plan. It only took me seven years!
I am currently revising all four documents due to a change in my marital status.
- Durable Power of Attorney
- Advance Health Care Directives, Medical Power of Attorney, or Living Will
- Will
- Trust
In this article, I focus on Advance Health Care Directives. These are important for caregiving families — care recipients and caregivers, alike. There are three important parts to this document for you to consider.
Times change. Our vocabulary changes. Health care advances mean we can better define various medical states. Greater knowledge and awareness of end-of-life care through hospice and other palliative-care options help us to better determine our own care choices.
For an overview of areas to consider, start with Five Wishes.
My original directives were completed in 2004. I began updating them in 2016. Then, all that would change due to an impending divorce after 40-plus years.
I’ve made it easy for you. I’m including the links I visit as I update my directives. To give you a sense of time, I’ve spent about 10 hours on my Advance Healthcare Directives. Do it in bite-sized pieces. Don’t try to finish in one weekend. You need time to think seriously about it between revisions. BUT don’t go too far. Commit to your decisions in your life as of today. Yes, you may change your choices, but write down the best decisions for you, today. In case of an emergency, you want people to know what you desire. They’ll need this information to make the right decisions about your care.
Choose Your Healthcare Agent
TIPS from the National Hospice and Palliative Care Organization on selecting a person and back-up. This should be someone who –
- Knows you well
- Is calm in a crisis
- Understands how you would make the decision if you were able
- Is not afraid to ask questions and advocate to doctors
- Can reassure and communicate with your family.
Provide Healthcare Instructions
While the basics are covered in these documents; you know you’re different. I certainly am! How I want to be cared for near the end of my life’s journey will be different than your desires. It’s important that you determine your own goals. Yes, you may shudder at the thought of planning for your end of life, but you’ll have a better chance of your desires being fulfilled. For example, do you want to prolong your life at all costs? I don’t! I choose quality of life.
In my advance health care directives, I added special instructions to help those caring for me know what I want, when, where, and even the kind of music I’d like along with how people should interact with me. I also included two items (abridged), which I will share here.
We equate eating with love. Yet, our bodies will begin to shut down during the dying process… I may not want to eat for up to 2 to 3 weeks or drink for up to 72 hours before passing. Allow my body to expend energy only where it needs to — for example, supplying blood to my major organs. There may not be enough blood going to my neck and stomach muscles to enable me to swallow and digest food without choking or worse. Please place an ice chip or two in my mouth for comfort from dryness.
Please do not use my condition for religious, political, or financial gain or to advocate an organization’s mission. Allow me to go with dignity and in peace.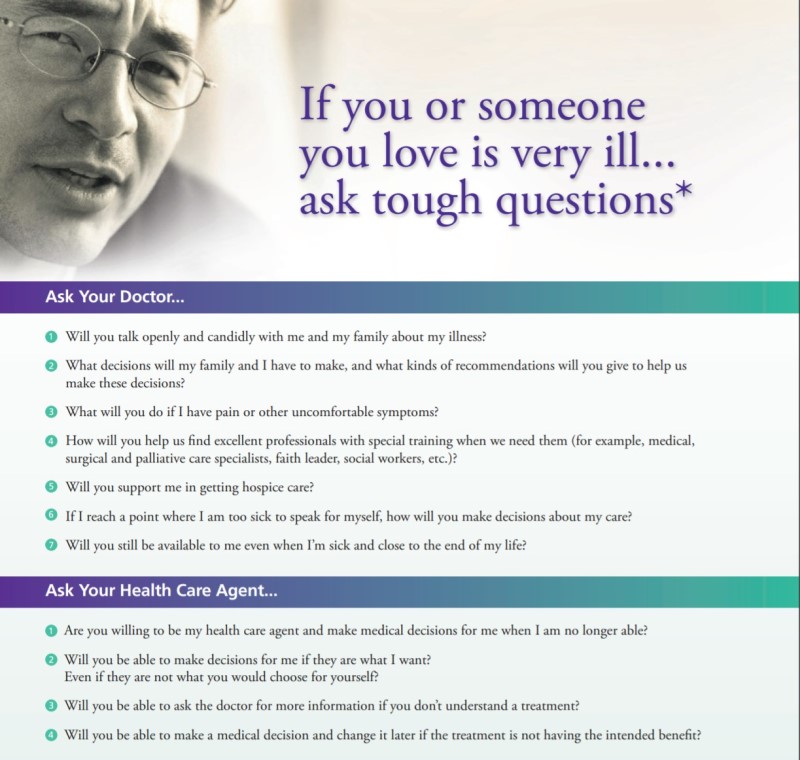
Guidelines for having these conversations — be sure to click on Ask Tough Questions to Professionals, Family Members, Spiritual Advisors, Lawyers [TCV Update 9/11/2024: URL now denies access to NHPCO page] Have regular conversations — a bit at a time. You want to be prepared when a crisis occurs. People can then act decisively on your behalf.
My father and I had regular conversations like these from my childhood into adulthood. He was 49 years old when I came into this world. I was curious and he replied candidly. During the last five years that he lived with Alzheimer’s, I remained confident in the decisions I made on his behalf.
Organ, Parts, and Tissue Donation
The third part gives you a choice as to whether you wish to donate your body or parts after death for transplant, therapy, research, or education.
Sign and Share Copies with Your Agent and Healthcare Providers
Once you’re finished and have signed the form, share with those named and the medical providers in your area, so they can be aware of your wishes.
You never know when an unexpected health emergency requires a life-and-death decision. Your family might be in shock and unable to decide.
For more information, contact —
Caring Info, a Program of the National Hospice and Palliative Care Organization
[7/18/2024 TCV Update] The page that opens to “Types of Documents to Make Healthcare Wishes Known: Advance Directives, Living Wills, PoAs, DNRs and POLSTs.” Being aware is an important first step in informed planning.
Links on this main page and along the sidebar will give you everything you need to get started on Documents, Fact Sheets, Glossary, and Resources.
For overview information regarding your Advance Directives for Healthcare. [7/19/2021 URL updated]
You can download your state’s Advance Directives thanks to CaringInfo, a program of the National Hospice and Palliative Care Organization.
When your or your care recipient’s healthcare needs necessitate these, here is a link to the Do Not Resuscitate (DNR) and Physician Orders for Life-Sustaining Treatment (POLST) forms. These are for the State of California. Your state may have different requirements.








