People with Alzheimer’s and other cognitive impairing diseases often say, “I want to go home.”
ASK TCV
My father who is in the middle stages of Alzheimer’s keeps saying, “I want to go home.” Then he starts walking out the door. How do we handle this situation?
TCV ANSWERS
Needing to “go home” means different things to people with Alzheimer’s.
It could mean his childhood home where he was comforted when he was afraid or hurt.
It could mean his early adulthood home that he shared with your mother.
He could also be feeling lost today and yearning for the comfort he remembers of his earlier years. As the disease destroys more of his brain cells, the reality of his existence — what he “sees” and “feels” often blurs.
Three steps to help your father feel better about “going home.”
- Learn about where “home” is for him. Encourage him to talk about “home.”
- Assure him that you will help him to return home. Walk with him and invite him to describe his home. Let him lead the way. Or take a drive and ask him to give you directions. Finish the trip with a fun outing for ice cream or tea or coffee with dessert).
- Supporting him in his quest to “go home” will comfort him because he knows he has an ally in his attempt to go home.
As the disease continues taking away pieces of your father, he will progress through this stage and forget about needing to go home.
Until then, my heart goes out to you.
Brenda Avadian, MA
Alzheimer’s / Dementia Caregiver, Expert Spokesperson, Coach, and Author
![]()
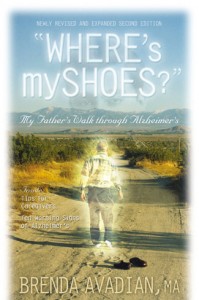
* My father’s desire to go home was so great, he “escaped” and was found walking along the freeway in the Mojave Desert. The story is told in “Where’s my shoes?” in The Great Escape chapter.
For additional info, click on and read: How can I handle my mother when she has hallucinations while saying she wants to “go home”? [8/29/2025 TCV Update: Caring.com URL no longer available.]









Hello, I once sat with a person who cried out “Home, I want to go home” every night at 6:00. The staff had told them “this is your home.” And, in fact she had no home to which she could return, it had been torn Down.
I asked, as you recommended what you do miss about your home? Some people have told me this is your home.
It’s not my home, they said. It doesn’t smell like him home. There is no wallpaper on the wall. It’s the wrong color. What happened to my bed? Where are the magazines, the doiles. This is not my home.
How right she was, and how relatively simple it would have b een to provide here with these things the first moment she was here. Smell might have been a challenge. But when I walked up and down the hallways every room smell the same. Is that true for houses?
Because many consider us fading away, losing our minds, out of touch with reality, they don’t take the time to listen to enough, not nearly enough. We are simply and apparently lied to and told things that just aren’t true, or others assume are true for us when they aren’t. Caregivers become so concrete in their appreciation of us, they miss the forest of touching, listening, just being there, for the trees that have already been torn down – homes, cars, etc.
We don’t become stupid, just confused and forgetful. We don’t become insensitve to today, ourselves, our needs: We just have trouble expressing them and meeting them ourselves.
Richard
P,S, turns out 6 PM is when she regularly came home from work. True, she was never given any “work” to do in her new “home” (bingo is not work, not purposeful activity), but her internal clock still knew when it was time to “go home.”
[TCV Update 9/16/2018: Dr. Richard Taylor passed away July 2015 and his website at RichardTaylorPhD is no longer operational.]
Richard,
What a value your perspective gives us caregivers as we try to discern what its like to view dementia from the other side–from the side you stand.
Thank you for taking time to share your words of wisdom and for reminding us not to take the shortcuts so many of us try after awhile.
After all, as you so often say in your lectures around the world (I paraphrase): There’s a person in here! ME!
Again, thank you, Richard.
My husband has AD. His wanting to go home was always back to his parents home about 7 miles from here. Every time he ran off, he was headed in that direction and once even made it 5 miles of the way. We now have a double keyed deadbolt so he cannot get out and he is so advanced at this point that I don’t know where he would go.
Amazing, isn’t it? 5 miles. WOW.
You are smart to do a double-keyed deadbolt. Just be sure to hide the key right by that door in case there’s an emergency and you need to get out fast.
Thank you, Linda, for writing.
My mother is in a nursing home and she knows what home is…no doubt. She wants to back to her own home RIGHT NOW RIGHT NOW.
No amount of this pretend stuff will work in this situation. I hear it to often that the person with memory loss is stuck in the past wanting home of childhood.
If the person is in a nursing home, I’d assume they just don’t like it there and want to go HOME to their home, just as we would. “Get me out of this place…” is what she is saying. I tell her the truth…and that we now have to make the best of this place, take comfort in the little things we can do together here. Eventually, she comes to a place of understanding, well to resignation, then with a sigh, does “get off it.”
So be very aware what home is to them…you are right.
Carol, thank you for sharing your experience with this.
Each person’s experience, as you also point out, is unique and the important variable is to learn where “home” is.
Again, thank you for your comment.
I don’t have personal experience with Alzheimer’s, but I have had family members with sever bipolar disorder who have gone through periods of not knowing or understanding their surroundings. My grandmother used to get electric shock therapy when my mother was a girl. My mom always told me of one Thanksgiving when Grandma came home from the hospital and didn’t know where she was. She wanted to go “home” meaning to the hospital. It was very hard for my mom and her siblings to hear that at such young ages. The points that you made about how to help a person “go home” would have made it easier on everyone, I think.
Great post! Thank you for the advice and compassion.
Thank you, Erin for sharing this. These treatments were commonplace many years ago and we continue to learn how to handle loved ones with different mental illnesses and cognitive-impairing diseases.
Thank you for shedding light and helping caregivers gain a historical perspective on “going home.”